
Scaphoid Fractures & Nonunions
What is a scaphoid fracture?
The scaphoid is one of the eight wrist (carpal) bones.
A fracture (or break) of the scaphoid bone is the most commonly missed injury for two reasons:
-
There may be little pain or swelling
-
The initial x-rays are often normal.
Scaphoid fractures that are missed and not treated early are the major cause of wrist arthritis and significant loss of function in young men.

How do scaphoid fractures occur?
Most scaphoid fractures occur from an injury with moderate force involving a fall on an outstretched hand during contact sport or bicycle/motorcycle accident.

Scaphoid Fracture



What are the signs & symptoms of a scaphoid fracture?
-
Distal radius fractures in children usually occur at the growth plate (physis) as it is made of cartilage and therefore weaker than bone.
-
The most common is the Salter-Harris II fracture (below).
-
Salter-Harris I-IV fractures rarely cause growth issues if the fracture is reduced (put back in normal position).
Salter-Harris V is a very severe injury which may cause growth arrest (the radius stops growing). However, growth arrest can also be treated and usually does not cause more than 2cm of shortening.

Distal scaphoid
Scaphoid waist
Proximal pole

What are the types of scaphoid fracture?
Location
Scaphoid fractures are grouped according to the part of the scaphoid that is fractured (broken). The majority of fractures are in the waist of the scaphoid.
-
Distal scaphoid
-
Scaphoid waist
-
Proximal pole
Proximal pole fractures have a much higher rate of not healing.
Displacement
Fractures can be undisplaced (not out of position) or displaced (out of position).
Undisplaced fractures can often be treated without surgery.

Undisplaced scaphoid waist fracture
Displaced scaphoid proximal pole fracture

How are scaphoid fractures diagnosed?
History & Examination
-
A history of a fall and tenderness in the anatomical snuffbox suggest that a scaphoid fracture is likely.
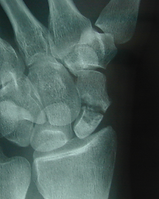
X-ray
-
An x-ray should be performed as the first test. However, the x-ray can be normal in ther first 2 weeks.
-
A repeat x-ray in 10 days should be performed and the wrist protected in a cast or splint.
-
If the x-ray remains normal, it does not mean that ther is no injury.
CT scan
-
CT scan will usually show a fracture if performed 3 days or more after the injury.
-
If the CT scan is normal and the symptoms persist, an MRI should be considered.
MRI scan
-
An MRI shows both bone and ligament injuries. MRI is not usually the first test for a scaphoid fracture as it is a more expensive test and not as readily available as x-ray or CT scan.

CT Scan Proximal Fracture

MRI Scan Scaphoid Waist Fracture
What is avascular necrosis and why can it prevent scaphoid fractures from healing?
The blood flow to the scaphoid enters the bone further from the wrist and travels back towards the wrist. When there is a scaphoid fracture, the blood flow can be disrupted. This can lead to the fracture not healing (non-union).
Avascular necrosis is when the blood flow to the scaphoid is disrupted by a fracture and cannot reach the proximal pole. The lack of blood supply to create new bone means that the fracture cannot heal.
Avascular necrosis is most common in proximal pole fractures which is why they have a high risk of non-union (not healing).
Avascular necrosis and non-union of the scaphoid are serious concerns and can lead to multiple surgeries being required, arthritis of the wrist and eventually the need for fusion of the wrist to relieve pain and weakness.

Blood flow to the Scaphoid
What are the treatment options for scaphoid fractures?
-
Cast only
-
Open reduction & internal fixation
Treatment will depend on many factors, including:
-
The location of the fracture
-
Whether the fracture is displaced (not in normal anatomical position)
-
How long ago the fracture occurred.
-
Whether there is avascular necrosis.
ALL suspected fractures should be immobilised. There is a higher risk of the fracture not healing if a cast or splint has not been applied in the first TWO weeks.
Cast treatment
The goal of treatment of any scaphoid fracture is to heal the fracture to relieve pain, return function and prevent arthritis.
-
Most simple fractures will heal with cast immobilisation for approximately 8 weeks.
-
Scaphoid fractures that have not been put in a cast or splint within 2 weeks of injury should be considered for surgery due to the high risk of non-union.


Scaphoid open reduction & internal fixation surgery
Surgical treatment of a scaphoid fracture is usually required for :
-
High energy injuries
-
Displaced fractures
-
Proximal pole fractures
-
Fractures that have not been put in a cast or cast within 2 weeks of the injury.
The procedure is a day surgery performed under general anaesthetic. The surgery involves a small incision of on the back or front of the wrist (depending on the location of the fracture).
A guidewire is placed across the fracture. X-rays are taken to confirm that the wire and the fracture are in the correct position. A screw is passed over the wire to hold the scaphoid in position while it heals. A bandage and temporary half-cast are applied.
A long-acting anaesthetic keeps the area pain-free for 6-8 hours. A prescription for pain relief and a sling will be be provided before being discharged from the hospital day surgery.
What is the recovery after scaphoid injury?
Recovery after cast treatment
-
Usually fractures take 8 weeks to heal
-
Physiotherapy is started once the fracture has healed and the cast removed.
-
Usually 3- 4 months until full movement has returned and unrestricted sporting activityis allowed.
Recovery after surgical treatment
2 days
-
Rest and elevation
-
Regular pain relief
-
Keep hand dry with cast protector or plastic bag
2 weeks
-
Temporary cast removed.
-
Sling should no longer be needed.
-
For fractures at low risk of nonunion, a removable splint and light exercises may be commmenced.
-
For more high risk fractures, a waterproof cast is required a cast for 8-12 weeks until fracture healing has been shown on progress CT scan.
2-3 months
-
Physiotherapy is gradually increased if fracture has healed.
3- 4 months
-
Full movement has returned
-
Unrestricted weight loading, manual work and sporting activityis allowed.
What are the risks & complications of scaphoid fractures?
-
Non-union (not healing) occurs in ~15% of scaphoid fractures, regardless of treatment. Non-union is more common if the fracture is displaced; the has been delayed treatment > 2 weeks; or the fracture is at the proximal pole where the blood supply is poorer.
-
Infection < 1%
-
Screw prominence requiring removal < 1%
-
Wrist stiffness
SCAPHOID NON-UNION
Scaphoid non-union (unhealed fracture) is a much more challenging situation and the outcome of surgery is not as good as treating a fracture soon after it has occurred. Unfortunately, as the symptoms are often not severe, many people do not have the fracture diagnosed until it has become an established non-union.
Thex-rays will demonstrate a gap in the fracture site, often sclerosis (whitening) of the fracture edges from rubbing against each other and cystic changes where the joint fluid and movement have eroded part of the scaphoid.
Iliac crest bone graft
Non-union of the “waist” or mid-section of the scaphoid can often be healed by clearing the fibrous, unhealthy tissue from the fracture site, packing it with a piece of bone-graft taken from the hip and inserting a screw to hold the fracture in position.

Vascularised bone graft
Non-union of small proximal pole have poor blood supply and may need to be treated with a vascularised bone graft, a bone graft moved to the scaphoid with its blood supply. This may be taken from the distal radius where a piece of bone is carefully moved with its blood vessels still attached or from the knee where the blood vessels are then attached to blood vessels in the wrist using microsurgery. (Image: vascularised graft graft from radius).

Scaphoid non-union risks and complications
In addition to the complication of scaphoid fractures, there are other risks for non-unions
-
Scaphoid non-unions are difficult to treat with a risk of requiring more than one surgical procedure to achieve fracture union.
-
If attempts to reconstruct the scaphoid with bone grafts/vascularised bone grafts fail, a partial or complete wrist fusion may eventually be required to manage pain and weakness.
-
Scaphoid non-unions are the most significant cause of wrist arthritis in young men.














