Base of Thumb Arthritis
What is Base of Thumb Arthritis?
In a normal joint there is a 2mm cartilage lining covering the bones which allows smooth, painless movement and acts as a cushion. When this cartilage lining wears out bone moves on bone. This age-related condition is osteoarthritis. Injury to the joint such as fractures that damage the joint lining or ligament injuries that cause instability can also result in arthritis. Inflammatory diseases such as rheumatoid and psoriatic arthritis also damage the joint and are known as inflammatory arthritis.
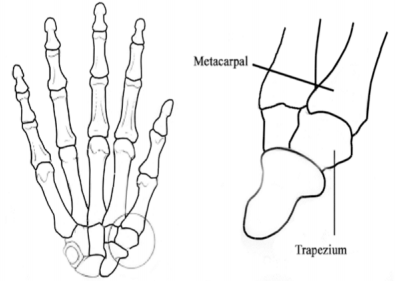
The joint at the base of the thumb is called the first carpometacarpal joint. A wrist bone called the trapezium and the first metacarpal bone form this joint. The unique ‘saddle’ shape of these bones allows enormous freedom of movement. Base of thumb osteoarthritis is far more common in women than men, and typically occurs after the age of 50. It is often hereditary.
What are the signs & symptoms?
 The earliest symptom of base of thumb arthritis is pain with activities that involve pinch. These include opening jars, door handles, car doors and turning keys. Repetitive grasping activities or heavy lifting may cause aching pain at the base of the thumb. Changes in the weather may also cause pain. As the arthritis gets worse, pinch and grasp become weaker and swelling and deformity of the joint occurs.
The earliest symptom of base of thumb arthritis is pain with activities that involve pinch. These include opening jars, door handles, car doors and turning keys. Repetitive grasping activities or heavy lifting may cause aching pain at the base of the thumb. Changes in the weather may also cause pain. As the arthritis gets worse, pinch and grasp become weaker and swelling and deformity of the joint occurs.
How is the diagnosis made?
Most patients will be aware of the signs & symptoms that have been described above. There is usually deformity/prominence of the base of thumb and tenderness. The ‘grind’ test is used to compress the joint and reproduce the pain. It may also produce a gritty sound called ‘crepitus’. This is due to bone contact against bone. Significant arthritis will be obvious on x-ray. Many patients with base of thumb arthritis will also have carpal tunnel syndrome. The carpal tunnel is narrowed by arthritis of the base of thumb and carpal tunnel syndrome is very common in women over 50 years of age.
How is base of thumb arthritis treated?
Non-operative treatment is often very effective in retired patients over 65 years. This includes:
1. A lightweight splint (Comfort Cool and/or Push-brace splint – hand therapist or online).
2.Panadol Osteo – 2 tablets 2-3 times per day
3. Short (5-7 day) courses of anti-inflammatories when symptoms flare up.
4. Exercises to strengthen the first dorsal interosseous muscle.
5. Modifying activities to minimize irritating the joint.
6. Modifying activities to minimize irritating the joint.
7. Steroid injections into the joint are rarely recommended as they give only temporary relief.
You may be referred to a hand therapist to assist in managing your arthritis. The aim of non-operative treatment is to provide you with the tools and knowledge to manage your arthritis so that it does not interfere with your lifestyle.
Surgery may be advised when non-operative treatment is not helpful. Active people in the 50–65-year age group are more likely to require surgery. Older people with lower demands often have excellent symptom control with non-operative treatment.


What does surgery involve?
The goal of surgery is to decrease pain and keep motion in the thumb. The procedure involves removing the trapezium bone (trapeziectomy) and using a wire suture material to stabilise the base of the metacarpal bone (suture suspension arthroplasty). It is performed under general anaesthetic and takes 60-90 minutes. The hand and wrist are immobilised in a bulky dressing with a fibreglass splint to protect the thumb. The splint will reach from your thumb to approximately 10cm below the elbow. The fingers are left free for light activities. An overnight stay is recommended for pain relief.
Risks
There is a less than 1% risk of infection and a very small risk of injury to skin nerves that may leave a small patch of numbness over the back of the thumb/hand. There is also a risk of less than 3% of the thumb metacarpal collapsing into the space created when the trapezium bone is removed which may require further surgery to re-suspend the thumb. Approximately 1 in 1000 patients who have hand surgery can develop a serious pain response that may require very prolonged rehabilitation and pain relief.
What about recovery?
Discomfort is expected in the first 3 months and improves with time. No strong grasp or pinch is allowed for 3 months to allow enough healing for stability of the thumb. It will take up to a year for the maximum benefits of surgery to be reached. Pain is greatly improved with surgery, but you may still have some occasional mild discomfort. Strength is usually also improved following surgery.
- 2 weeks: Bulky bandage & half cast from forearm to hand is removed. Changed to light weight splint.
- 4 weeks: Splint shortened to wrist level and physiotherapy commenced. Driving, typing, writing may recommence. (“Pen Again” is very helpful for writing.)
- 8 weeks: Light gardening, golf, bike riding etc with splint. No strong gripping or heavy lifting.
- 12 weeks: Activities unrestricted but may still prefer flexible splint for more repetitive tasks/sports.
- 6 -12 months: Maximum strength & pain relief.

